U of I Researchers Discover Cancer-Killing Drug
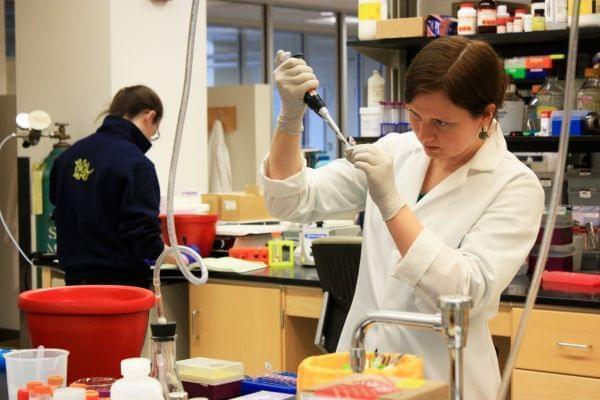
Rachel Botham, a graduate student at the University of Illinois, prepares solutions of proteins isolated from cancer cells that she treated with chemotherapy drugs. Botham has spent the past 5 years as part of a team working on the development of PAC-1, a new drug candidate for the treatment of brain cancer. Credit: Christine Herman
It's been just over a year since Brenda O’Brien brought her fiancé Pete Biondo to the emergency room at Mercy hospital in St. Louis. She thought he had a tooth infection. But it turned out to be something far more serious.
“They saw a tumor,” she said. “The next day they went in and did a biopsy of it, and they told us that it was anaplastic astrocytoma.”
A terminal form of brain cancer.
The tumor—which was the size of a grapefruit—was too large to be operated on. The doctors said Pete could expect to live another 7 to 10 months.
“I was devastated,” O’Brien said. “You just don’t expect that. So, it was shocking, and it took about, I guess, two days, to really let it sink in.”
Pete has outlived his prognosis by about 5 months. But the illness, the aggressive treatments involving radiation, chemotherapy and drugs to manage side effects, have taken a toll.
“There would be a delay in his thinking, he didn’t function for himself,” O’Brien said. “He had to have somebody live with him to make sure he ate something, make sure he did take showers… It’s been, you know, just a rollercoaster of a ride because at one point you think he’s dying and then the next couple months he seems to turn around, and the cycle starts all over again.”
Pete Biondo shares a laugh with his grandson Caidan last summer at his home in St. Louis, Missouri. Caidan was born two days prior to Pete’s diagnosis of anaplastic astrocytoma, an aggressive form of brain cancer.
Credit: Christa Busse
Some 22,000 people in the United States will receive news like Pete’s this year. And roughly 15,000 will die from cancers of the brain and nervous system. That's nearly 3 percent of all cancer deaths, according to the American Cancer Society. For a patient with the most aggressive form of brain cancer, known as glioblastoma, the future is bleak.
“Without treatment, median survival is 3 months,” said Paul Hergenrother, a professor of chemistry at the University of Illinois. “With treatment with radiation, it’s 12 months.”
At best, coupling radiation with chemotherapy drugs can add another couple months to a patient’s life expectancy. “Obviously still very grim prognoses for these patients,” he said.
But Hergenrother is working to change the prognosis. Researchers in his lab screened thousands of molecules and discovered one that showed promise in fighting cancer. They called it PAC-1. The compound is now in the early stages of testing in humans. This week, the first patient will receive the experimental drug as part of Phase One of clinical trials—the first of three stages of testing in humans mandated by the US Food and Drug Administration before a drug can enter the market.
PAC-1 is not like most chemotherapy drugs. It can cross the blood-brain barrier, the network of cells that acts as the gatekeeper between the brain and the rest of the body.
“We’ve developed sophisticated mechanisms to keep things out of the brain,” Hergenrother said. “And that’s, in general, a good thing with respect to dietary intake and environmental toxins.”
But it makes it particularly difficult when you want to get a molecule, like an anti-cancer drug, into the brain to attack tumor cells.
“Some 98 plus percent of drugs do not get into the brain,” he said. “And most all of cancer drugs do not get into the brain.”
So Hergenrother says it came as a surprise when they realized PAC-1 made it through. It wasn’t even a characteristic they were looking for when they set out a decade ago to discover new anti-cancer drugs.
“It was discovered as part of an effort to think about novel cancer targets and try to find drug candidates that hit those novel targets,” he said.
The novel target in this case is an enzyme known as procaspase-3. Many forms of cancer have higher-than-normal levels of the enzyme, which when activated, triggers a series of events that ultimately destroys the cancer cell. Hergenrother hypothesized that a molecule that activates procaspase-3 would be an ideal drug candidate. By turning the cancer cell against itself, it would kill those cancer cells and leave healthy cells unharmed. Some of the earliest experiments with PAC-1 suggested he was on to something.
“We showed that it potently induces death in cancer cells in culture and in cancer cells taken from patient samples,” he said.
When they later discovered PAC-1 could penetrate the brain, they worried about the risk of neurotoxicity – a side effect that can damage nerve cells and brain tissue. But they figured out that they could reduce neurotoxic effects by giving the drug as a pill, instead of through an IV. These studies of PAC-1, performed in mice, rats, and dogs, were done in collaboration with Dr. Tim Fan, a veterinary oncologist at the U of I.
“The initial concern about PAC-1 having the ability to get into brain, which we originally thought was perhaps undesirable, has come full circle to say how can we exploit that property and actually use it to our advantage,” Dr. Fan said.
Namely, to treat brain cancer. Over the past several years, the team has tested PAC-1 in animals with different types of cancer. They compiled the data to send to the FDA for evaluation. Then in February, they received approval to move forward with clinical trials in humans. Those are now being conducted at the University of Illinois at Chicago with patients diagnosed with many different cancer types for whom standard therapies have proven ineffective. Dr. Oana Danciu, assistant professor of medicine at UIC, is managing the clinical trial.
“Our goal with these early phase studies is to determine the dose that is tolerated by a patient safely,” Dr. Danciu said.
The next step will involve the recruitment of patients with primary brain tumors for a similar set of safety tests. If all goes well, Hergenrother says they will evaluate PAC-1 on a larger number of brain cancer patients, comparing the outcomes of those who receive standard treatments with those who receive standard treatments plus an added dose of PAC-1. Preliminary studies have shown PAC-1 works in combination with other drugs to kill more cancer cells.
“I really think this is the future,” Hergenrother said. “We want to be able to add PAC-1 to these preexisting regimens, and based on all our cell culture and preclinical animal data, that seems to be a very effective and synergistic strategy.”
It may be years before we know whether PAC-1 will be able to treat brain cancer in humans without debilitating side effects. Clinical trials vary in cost and size but can easily last about a decade and cost tens of millions of dollars to complete. And roughly 90 percent of drugs that begin clinical trials do not ultimately make it to the market for one reason or another.
Back in St. Louis, Brenda O’Brien continues to care for her fiancé Pete Biondo, keeping an eye out for signs that his cancer is worsening. Next month, they’ll go back to the hospital for another MRI to check on Pete’s brain tumor, which has neither grown nor gotten smaller since his treatment began. Brenda, says there’s an urgent need to continue to develop new treatments like PAC-1 so that patients like Pete can have a fighting chance.
“This disease is not gonna go away,” she said. “It’s just devastating to know that there are not a lot of options out there for you.”
For brain cancer patients today, this is the unfortunate reality. But it’s something that researchers hope will soon change.

