Feds OK Illinois Expansion of Medicaid Mental Health Coverage
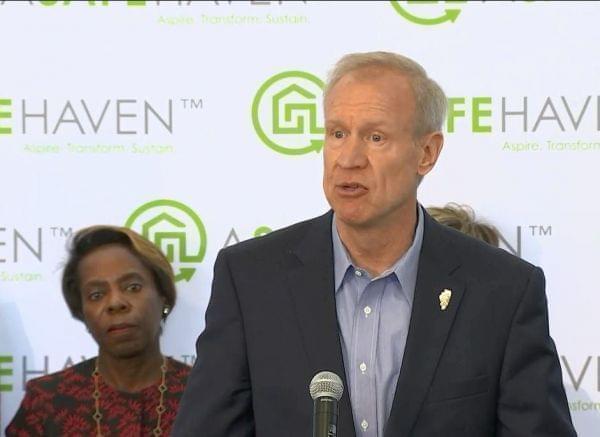
Gov. Bruce Rauner announces the new program at an event in Chicago on May 7, while HFS Director Felicia Norwood, left, looks on. Illinois Central Management Services
lllinois' three million Medicaid users will soon have more access to mental health and substance abuse treatments. Officials in Washington, D.C. okayed a new state program that sets aside about $2 billion in Medicaid funds for the services.
If you’re someone who uses Medicaid, you’re covered if you go to the doctor’s office or hospital when you get physically sick. But if you have a mental health issue like depression, for example, and want a counselor to come visit you at home, it’s a different story.
Healthcare and Family Services Director Felicia Norwood says that’ll change with the new program. Money will now be set aside to help people pay for things like in-home counseling and even addiction recovery.
“Mental health, behavioral health is something that impacts everyone in our state. It knows no geography, young and old.”
The move is part of the Rauner administration’s effort to spend Medicaid dollars on less-expensive outpatient services. Governor Rauner himself says expanding those kinds of treatments will set the state apart.
“We’re gonna become national leaders in the way mental health services are provided to the residents of our state," he explained. "We’re gonna become much more proactive in preventive health services and community-based health services.”
The administration says Illinois spends more than 50 percent of its Medicaid budget annually on people who need mental health treatment. The new program, called Better Care Illinois, will cover treatments in 10 different pilot programs as early as July.
Links
- Medicaid Cuts Hurt Independent Pharmacy Owner
- Small Pharmacies Hit By Medicaid Cuts; Solitary Confinement; Illinois’ Endangered Places
- Time For Medicaid Recipients To Choose A Managed Care Plan
- Rauner Vetoes Medicaid Purchase Plan As Duplicative
- Illinois Medicaid Providers Still Struggling; Cairo Responds to Secretary Carson’s Visit
- Medicaid Bill Backlog Pushing Illinois Doctors To The Brink Of Closure
- Pritzker Wants to Let Anybody Buy into Medicaid

