How A Kansas Hospital Survived Multiple Owners And Bankruptcy

Hillsboro Community Hospital, then known as Salem Hospital, was housed in this building that opened in 1953. Dan Margolies/KCUR
Nine months ago, things were looking bleak for Hillsboro Community Hospital, a 15-bed facility in central Kansas about 50 miles north of Wichita.
The critical access hospital appeared to be facing the same fate as four other rural hospitals in Kansas that have closed over the past three years.
Its lender, Bank of Hays, had foreclosed after the hospital defaulted on a $9.6 million construction loan. The city, which had floated revenue bonds to help construct a new building just two years earlier, was threatening to shut off the hospital’s electricity after it fell behind on its utility bills.
Perhaps most ominous of all, the hospital’s owner, Empower HMS, had missed payroll, supplies at the hospital were running low and hospital employees were reduced to holding fund drives just to feed the hospital’s patients.
“In the period from November 2018 through about the 10th of January of 2019, the hospital was essentially in abandoned condition,” says Brent King, who was appointed bankruptcy trustee after the hospital filed for Chapter 11 protection in March. “No bills were being paid, employees’ wages were often not being paid.”
In 2017, the hospital had every reason to think its future was bright. The gleaming new building, which cost $11.4 million, replaced an aging facility that opened in the early 1950s. It was the fifth iteration of the hospital, whose forebear was established in 1893 to serve Hillsboro, a farming community founded by Russian and Ukrainian Mennonites in the 1870s.

The now-vacant building that housed Hillsboro Community Hospital from the early 1950s to 2017.
With about 2,900 residents, excluding 750 students at local Tabor College, the town boasts two trailer manufacturers and is the headquarters of one of the nation’s top honey producers, Barkman Honey, which set up shop there in 1960. Hillsboro Community Hospital, with about 75 or so full- and part-time employees, was among the largest employers in town.
But around the same time the hospital moved into its spanking new quarters, a private company run by a group of Florida businessmen took it over. The group, Empower HMS, had loaned money to the previous private ownership group, and when that group defaulted on the loan, Empower exercised an option to acquire its stock in the hospital.
Hillsboro was one of 18 financially distressed hospitals in eight states that Empower ended up taking over. The company promised to turn them around through a lab billing arrangement that took advantage of the higher rates paid to critical access hospitals, which are small rural facilities that are entitled to cost-based reimbursement from Medicare.
But Empower’s promises proved empty. Soon after it began running Hillsboro, bills began piling up, the bank filed its foreclosure action and the city said it would turn off the lights if the hospital didn’t pay its delinquent utility bills.
Things got so bad that in January, a state court judge appointed a receiver to take over and run the hospital. “Immediate and irreparable harm is likely to result if a receiver is not appointed to operate and manage the Hospital in order to ensure that it remains open and retains as much of its value as possible,” the judge wrote in his ruling.
The receiver, Cohesive Health Management + Consulting LLC of Shawnee, Oklahoma, in turn placed the hospital in Chapter 11 bankruptcy.
It was a troubling and uncertain time for the hospital, its employees and the community.
“I would say it was very disheartening,” says Olivia Robinson, the bank’s human resources manager, speaking of the months leading up to the bankruptcy filing. “Employees felt they did not matter, that they were a dollar sign and because that dollar sign had run out, they were no longer needed – kind of thrown to the side as trash.”

Olivia Robinson (left), the hospital’s human resources specialist, with Miranda Reed, a physical therapist assistant.
Empower, led by a Miami businessman named Jorge Perez, promoted itself as a savior of troubled rural hospitals. Perez claimed to have discovered the “secret sauce” that would turn their fortunes around.
Empower took advantage of the higher reimbursement rates the federal government offers to critical access hospitals, which allows them to bill for laboratory tests at higher rates than other medical providers.
“Part of our secret sauce is that we will bring in new services that didn’t exist before,” Perez said in a September 2017 interview after announcing that Empower had acquired Fulton Medical Center in Fulton, Mo., another hospital on the brink of closure.
Except that Perez and his associates billed insurers for urine and blood tests drawn for thousands of patients who had never so much as set foot in any of their hospitals. The scheme began to unravel in August 2017, when Missouri State Auditor Nicole Galloway accused Empower and Perez of using tiny Putnam County Memorial Hospital in north central Missouri as a vehicle to shunt much of the money from its lab billing scheme to Perez and his business associates.
Over a nearly 10-month period, according to Galloway’s audit, Putnam County Memorial Hospital received more than $90 million in insurance payments for lab work that was conducted for patients who had not been treated at the hospital. Instead, Galloway said, Putnam County Memorial Hospital served as a shell company for other labs by submitting bills for their services and funneling the insurance payments through the hospital.
Insurers eventually wised up to the scheme and stopped paying, marking the beginning of the end for Empower and, by extension, many of the hospitals it owned and operated.
Now Empower and Perez are under criminal investigation by federal and state authorities, according to court filings. Perez, who could not be reached for comment, told KCUR in the fall of 2017 that the lab billing arrangements were perfectly legal and a way to ensure the long-term survival of rural hospitals teetering on the edge of insolvency.

Inpatient room at Hillsboro Community Hospital.
But King, Hillsboro’s bankruptcy trustee, said he and his associates uncovered massive billing irregularities at another Empower-operated and now-shuttered hospital in Graceville, Fla. King told KCUR in April that after Perez and his associates took over the management of Campbellton-Graceville Hospital, its lab billings somehow shot up from $13 million a year to $130 million a year.
Today a dozen of Empower’s hospitals are in bankruptcy and eight have closed. But unlike the other bankrupt hospitals, whose fates remain tied to Empower, Hillsboro – by ousting Empower under the aegis of its court-appointed receiver – has managed to control its own fate.
That – along with an outpouring of support from the community – has made all the difference in terms of its prospects for survival.
“You know, there are specific things for small communities that they need to be successful,” says Hillsboro City Administrator Larry Paine. “Hospitals, schools, post offices, you know, churches, those sorts of things. When you don't have those, you are on the decline.”
The hospital was just days from closure when Cohesive, the receiver, brought in Margaret Grismer, a U.S. Navy and Public Health Service veteran, to run it. By then, the hospital lab had shut down, the emergency room was diverting patients elsewhere, and the hospital supply room was practically empty.
The first thing Grismer did was reopen the lab, find pathologists to run it and secure needed supplies. Then she reopened the emergency room.
“Having a functioning lab in a hospital is indispensable to the hospital’s and other operations, but particularly the emergency department,” Grismer explains.

Margaret Grismer, a U.S. Navy and Public Health Service veteran, was brought in to run the hospital earlier this year.
Now, less than a year later, Grismer is hopeful the hospital will not just survive but thrive.
“We’ve had daily and weekly checkups from the city administrator and the mayor and the folks at Tabor College and the community, which just continues to utilize the facility and give us their daily support and cheer us on,” she says.
There’s little question that rural hospitals are struggling – even critical access hospitals, which qualify for special treatment by the government. Since 2010, 113 rural hospitals nationwide have closed, including 16 this year. Another 673 are vulnerable to closure, according to a study sponsored by the National Rural Health Association.
Forty-six percent of rural hospitals nationwide are losing money on operations, according to the association. In Kansas, one of 14 states that have not expanded Medicaid, a staggering 86 percent aren’t profitable.
“It’s a combination of multiple factors,” says Brock Slabach, the association’s senior vice president for member services. “Lower inpatient volumes, that’s one. Second is reimbursement declines. It’s just a different dynamic these days.”
A study by the U.S. Government Accountability Office last year said that rural hospital closures generally were preceded and caused by financial distress. That distress, it said, was due to multiple factors, including the higher percentage of elderly residents in rural areas, the higher percentage of residents with chronic conditions, lower median household incomes, decreasing populations and slow employment growth.
When a rural hospital closes, a cascade of problems typically ensues. There are the lost jobs and ripple effects on contractors and vendors. Sick people have to travel greater distances to get care. Doctors and other medical providers leave town. The town’s appeal as a place to live is diminished.

A look down Main Street in Hillsboro, Kansas.
“The importance of hospitals to rural communities goes well beyond health care,” says a recent issue brief by the Alliance for a Healthy Kansas, a group advocating for Medicaid expansion in Kansas. “Hospitals are among the largest employers in their communities and serve as local economic engines, creating jobs and attracting and supporting businesses and residents.”
The impact of a rural hospital’s closure often makes itself felt in less tangible ways as well.
A recent University of Washington study found that mortality rates increased by nearly 6 percent when rural hospitals in California closed. The reasons are not entirely clear, and further study is needed to determine if the California results apply to other states. But “there is a need to pay closer attention to what’s going on in rural areas,” says study co-author Krittee Gujral, a postdoctoral fellow at the University of Washington.
Gujral offers several possible reasons for the uptick in mortality following a rural hospital’s closure: the longer time it takes to transport a patient to another hospital; transportation barriers such as not having a car; and overcrowding at neighboring hospitals resulting from the closure.
“So it’s certainly a bigger concern that the people most affected by the closures are going to be people that have greater travel barriers, greater transportation barriers,” Gujral says. “And that often tends to be either low-income groups or the elderly, who are maybe less willing to drive, less able to drive, etc.”
King, Hillsboro’s Chapter 11 trustee, has no doubt that, whatever effects it may have had on mortality rates, shutting down Hillsboro Community Hospital would have had ruinous effects on the community.
“We know that parents who want to send their children to college in a town like Hillsboro, Kansas, one of the first questions they're going to ask is, ‘What about health care?’” he says. “‘What if my kid gets sick? Where’s he gonna go?’”
While the reasons for rural hospitals’ plight are varied, they’re tied to the plight of rural America in general: declining populations, shrinking employment growth and high uninsured rates. Plus rural residents are likely to be older, poorer and have higher rates of chronic illness than those living in more urban areas.
Hillsboro faces many of the same inexorable pressures, yet somehow has managed to stay afloat.
It’s not clear why the hospital has managed to survive while others have closed. But experienced and competent management and the community’s all-out support seem to be two key factors.
“I’ve seen some really well-performing hospitals where you’d never expect that, kind of like flowers growing out of a rock,” says Slabach of the National Rural Health Association, himself a former hospital administrator. “And I’ve seen hospitals in towns of 12-, 15,000 people that are closing or are on the rocks because they have bad management or bad boards or both.”
He adds: “It’s kind of like the barn has burned and so now we’ve got to come together and see what we can do to fix it. And so everybody is pulling in the same direction. That’s a really important factor as well.”
City and hospital administrators also point to how the town and hospital have pulled together to keep the doors open.
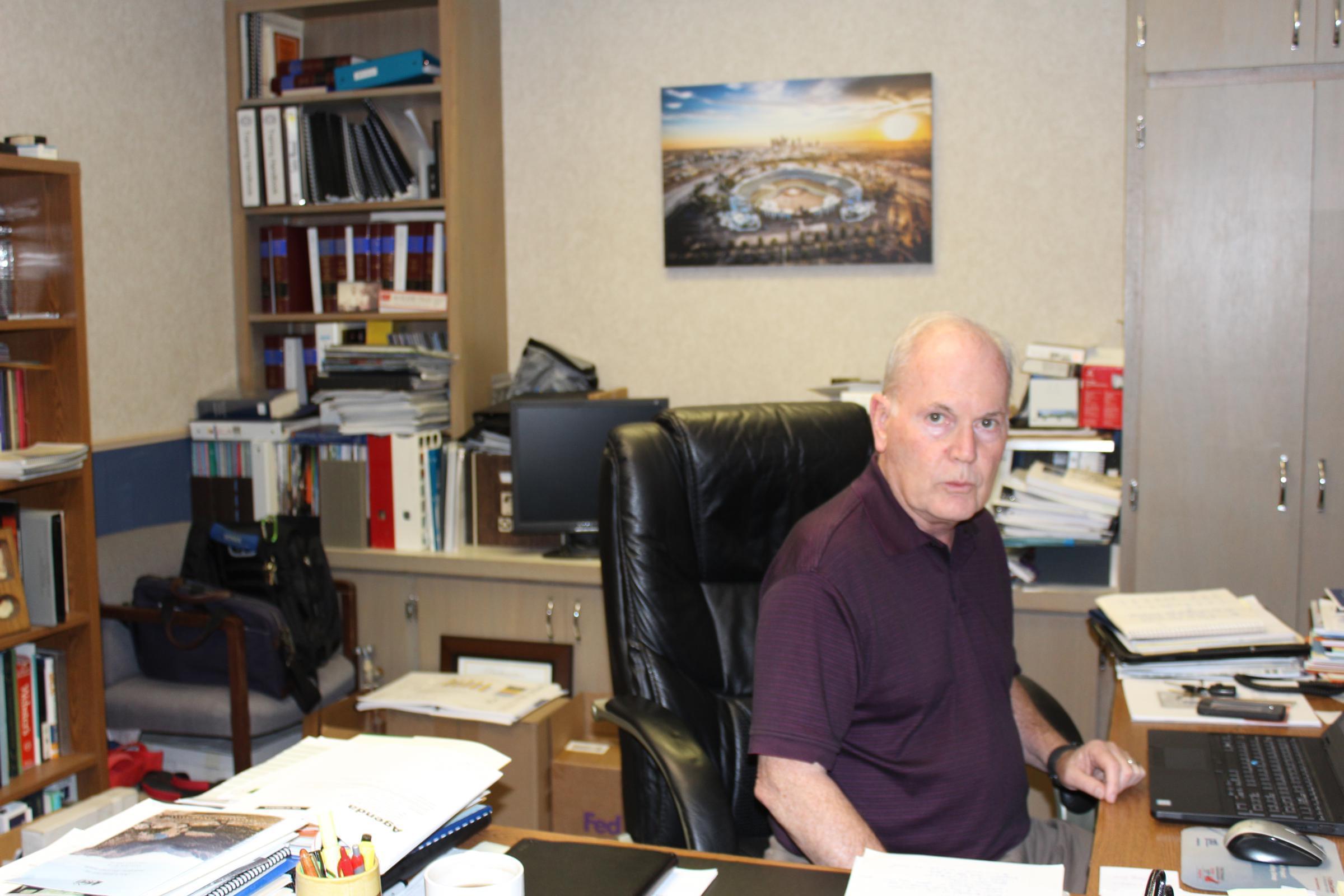
Larry Paine is the city administrator of Hillsboro.
“From a city manager’s point of view, you don’t ordinarily get thank yous for doing risky things,” says Paine, the city’s administrator.
“Being a partner with all the various people that are doing work to keep that place open – you know, it’s not just Larry, it’s the whole city council, it’s the bank, it’s the trustees, it’s the legal staff that we’ve got that’s making all the difference.”
Whether that outpouring of support is enough to overcome the demographic and economic forces that have led to the closure of other rural hospitals remains open to question. But so far, the doughty little hospital has managed to defy the odds.
Dan Margolies is a senior reporter and editor at KCUR Public Media in Kansas City, Missouri. You can reach him on Twitter @DanMargolies.
Seeking a Cure: The quest to save rural hospitals is a collaborative project including the Institute for Nonprofit News and INN members IowaWatch, KCUR, Bridge Magazine, Wisconsin Watch, Side Effects Public Media and The Conversation; as well as Iowa Public Radio, Minnesota Public Radio, Wisconsin Public Radio, The Gazette (Cedar Rapids, IA), Iowa Falls Times Citizen and N'west Iowa REVIEW. The project was made possible by support from INN, with additional support from the Solutions Journalism Network, a nonprofit organization dedicated to rigorous and compelling reporting about responses to social problems. For more stories visit hospitals.iowawatch.org

