Why Rural Hospitals Keep Closing Maternity Wards

Jessica Sheridan, 27, was seven months pregnant when she found out Hansen Family Hospital was considering closing their labor and delivery unit. Natalie Krebs/Side Effects Public Media
Jessica Sheridan’s plan was to have her first daughter at the local hospital, five minutes from her house in Iowa Falls. But when she was seven months pregnant, that plan suddenly changed.
“I think October is actually when we learned that the labor and delivery unit was talking about closing,” Sheridan said. “Obviously, we were, like, kind of in a panic. We’re like, ‘Oh my gosh, like, what are we going to do?’”
For Sheridan, this meant that the nearest hospital to deliver Arya was 45 minutes away in the small town of Clarion.

The Hansen Family Hospital in Iowa Falls, Iowa, stopped delivering babies last November. Hospital officials cited declining births, rising costs and the loss of a family doctor who did most of the deliveries as reasons.
As her due date neared, she fought to keep the rural unit open in Iowa Falls, a community of just over 5,000 in the central part of the state. She delivered a petition with 800 signatures to hospital officials, but Hansen Family Hospital closed the unit in November.
“I really genuinely believe that, that nobody was happy. Nobody at the hospital. It was ... something that was inevitable, I guess,” she said.
The closure sent Sheridan scrambling -- just two weeks before her due date. Instead of delivering with her local doctor, Sheridan started traveling to a hospital in Ames, an hour away.
“We had to do all of our remaining visits in Ames to kind of get to know those doctors down there,” she said, “because there's multiple labor and delivery doctors that deliver down there.”
Sheridan delivered Arya in mid-December. Though she said she was pleased with her experience at the Ames hospital, she and her husband still worried about the winter weather leading up to the due date.
“We were lucky. It was nice weather,” Sheridan said.
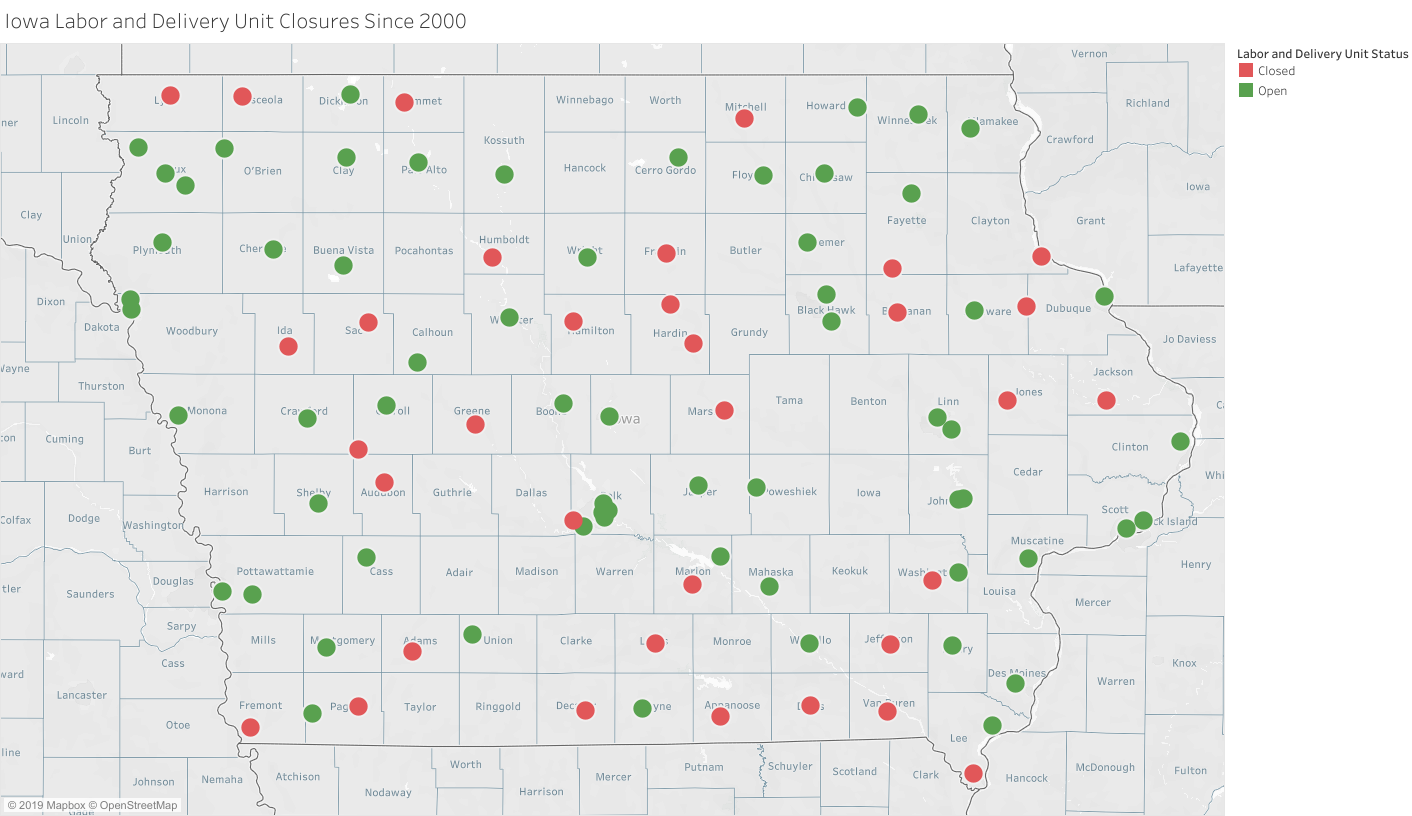
Nearly three dozen rural Iowa hospitals have closed since 2000.
‘A perfect storm’
Hansen Family is hardly the only hospital facing this tough choice. In the past two decades, nearly three dozen small Iowa hospitals have stopped delivering babies. Hansen Family was one of eight hospitals that stopped delivering last year, the most in one year, according to records from the Iowa Department of Public Health.
Last month, Unity Point Hospital in Marshalltown became the most recent hospital to announce it will stop delivering babies when it closes its unit this September.

Hansen Family CEO Doug Morse said the hospital held meetings with the public and stakeholders when it was considering closing the unit.
Officials at Hansen Family decided that labor and delivery care was too expensive for an aging, rural community with a declining birth rate, said CEO Doug Morse.
“One of the hardest lessons that we learned as a community was to deliver those 86 babies, this hospital was losing nearly a million dollars,” he said.
Morse says after three months of public meetings, hospitals officials opted to use half the money they would save to turn the unit into a mental health program for seniors.
“It really did become fairly clear that people recognize that this wasn't necessarily -- delivering babies isn't necessarily a service that matches an elderly population,” he said.
Iowa’s aging population is a key reason for these closures, said Stephen Hunter, vice chair of obstetrics at the University of Iowa Hospital in Iowa City.
“Some rural counties have lost as many as 40 percent of their population in the last three decades,” he said. “That's a lot of people gone, unfortunately, that leaves a system that's not adequate for those that remain in those counties, and areas.
Hunter said there are several other reasons that contribute to closures -- what he calls a “perfect storm.”
“Medicaid reimbursements are so low for OB that hospitals can't survive,” he said.
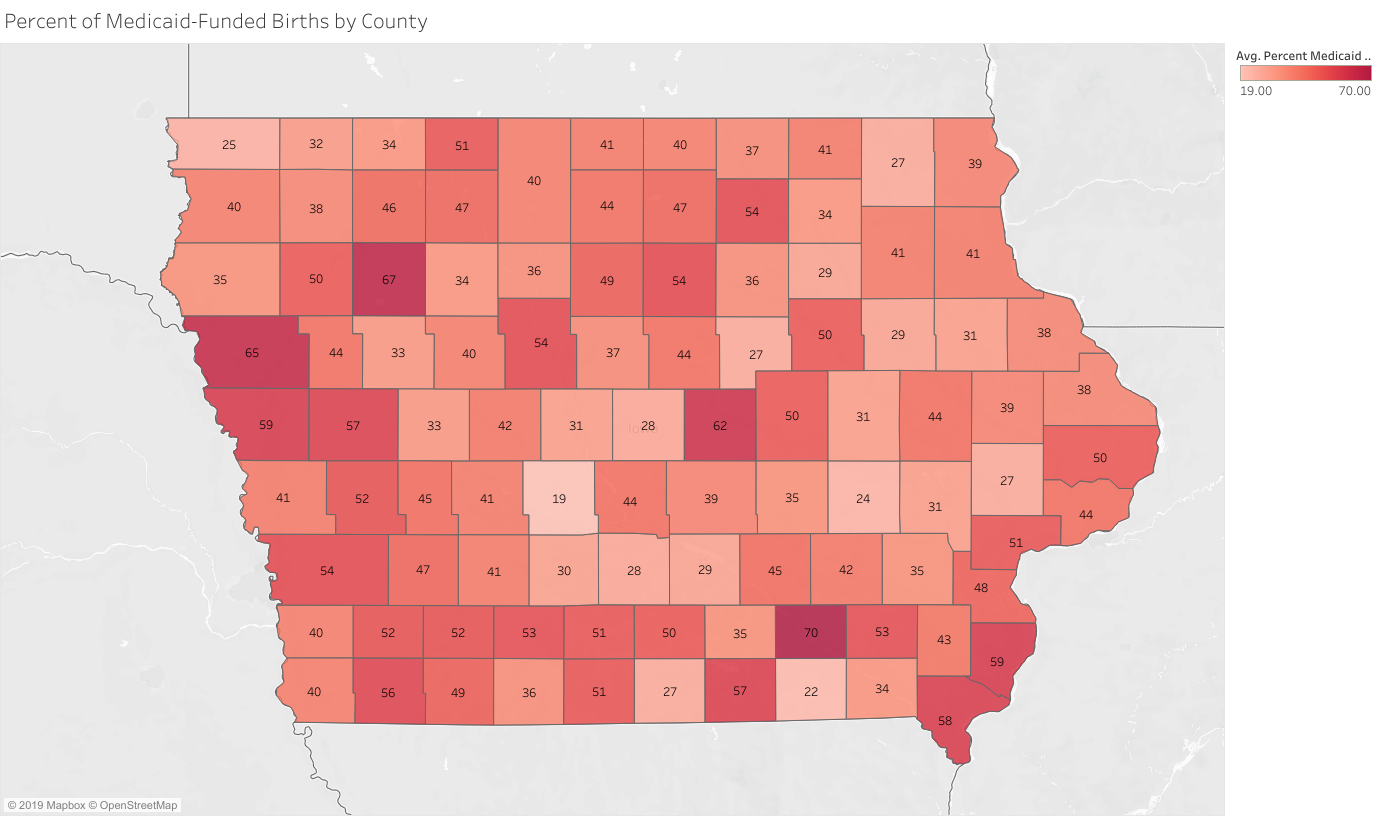
The percentage of Medicaid-funded births by Iowa county in 2018.
According to numbers from the University of Iowa, Medicaid -- government-funded insurance for those with low incomes -- reimbursed its hospital about a third of what commercial insurance plans did for services like ultrasounds and deliveries last year.
In Hardin Co., where Iowa Falls is located, 44 percent of births were Medicaid-funded in 2018, according to data from the Iowa Department of Public Health.
Hunter said the state is also facing a severe shortage of OB/GYNs and family practice doctors who practice obstetrics.
The state ranks 49th for the number of practicing OB/GYNs with only 1.49 doctors per 10,000 women according to the American College of Obstetricians and Gynecologists.
“Most of those OBs are practicing in urban areas, not rural areas,” Hunter said.
This was one of the factors that started Hansen Family’s conversation to close the unit last fall, Morse said.
The hospital’s family practice doctor, who was doing the vast majority of the hospital’s deliveries, left last November, he said.
“It became a system very much dependent on just a few people,” Morse said. “As we all know -- or maybe people don't know -- the being on call 24/7/365 to deliver babies in this environment is very difficult.”

Hansen Family Practice Doctor Thomas Waters is one of the doctors who helped the hospital come up with the “share care” model. Waters said many family physicians like himself no longer want to deliver babies.
Thomas Waters, a family practice doctor at the hospital, said there are many reasons why doctors, including himself, no longer want to deliver babies.
“It's a big lifestyle commitment to deliver babies," he said. “You're on call overnight and delivering babies then come into clinic the next day so lack of sleep.”
Waters said malpractice insurance rates are also higher for doctors who deliver babies.
But studies show there can be negative effects when rural communities lose obstetrics units.
According to a 2017 University of Minnesota study, the loss of labor and delivery units in smaller, more remote counties is linked with a decrease in prenatal care and increase in out-of-hospital and preterm births.
‘We have to look at it from a reality point of view’
At her office on a hot summer afternoon near downtown Iowa Falls, Diana Thies, the director of the town’s chamber of commerce, said the hospital is one of the pillars of the local economy.
That's one reason people do move here or decide to stay here is because there is a hospital,” she said.

Diana Thies, the director of the Iowa Falls Chamber of Commerce, said the Hansen Family hospital is an economic pillar of the community.
She was disappointed when hospital administrators approached her last fall with news that the labor and delivery unit would be shuttered, but understood the financial strain they were under.
“I also don't want to lose our hospital. So if taking one department out, and being able to financially -- the hospital thrive financially -- then I'm okay,” Thies said.
But she still worried it could take families away from local doctors -- and the local economy.
“I just don't want people to leave because will they come back and use our hospital? Will they come back and use our clinic?” Thies said. “Are they going to go, ‘just since I'm down there, I'm going there anyway, we'll just use those doctors, because now I'm familiar with them?’”
For Mayor Gene Newgaard, there was an emotional tie to losing the unit. He was born in Iowa Falls -- just like his mother and brother.

Iowa Falls Mayor Gene Newgaard said he understands why the hospital stopped delivering babies, but would like to see the service come back in the future.
“You think about the fact that, well, nobody going forward is going to -- unless it's an emergency -- is going to actually be born here,” he said. “You know, they're always going to say they're born somewhere else.”
Newgaard said while the news was a blow for the whole town, like Thies, he understood why hospital administrators made that tough choice.
“I think the community has, for the most part, accepted it,” he said. “Some may not still be happy about it, but we have to look at it from a reality point of view and making sure that our hospital is viable and continues to be here.”
Hansen Family’s Morse said following the public meeting last fall, the hospital opted to put a “share care” program in place once it stopped delivering babies.
Under the plan, women receive pre- and post-natal care in Iowa Falls. As they near their due date, they start planning for their delivery at Mercy One Medical Center in Mason City by meeting with the doctor, who meets with them in Iowa Falls, and planning the hour drive north to deliver.
“The idea is, you do as much as you can in a rural community, and then work with a referral center to partner and then come back to the rural community,” Morse said.

Molly Forgy, 27, of nearby Ackley, Iowa, had her son an hour away in Mason City last April using Hansen Family’s “share care” program.
Morse said initial figures show that under the system, three-fourths of women are bringing their children back to the doctor in Iowa Falls, instead of sticking with their out-of-town provider.
Molly Forgy of nearby Ackley was one of the first women to use the “share-care” program. She delivered her son in Mason City last April.
“I did not feel that I missed out on anything through having to go to two facilities and seeing two providers,” Forgy said.
But the hour drive north to deliver is a strain on others.
At eight months pregnant, Nicole Grover said she’s nervous about travelling so far because, four years ago, Iowa Falls doctors delivered her daughter by emergency C-section.

Nicole Grover, 32, and Jessica Lara, 44, were both upset about the hospital’s closure. Grover has to travel an hour away to Mason City to delivery and doesn't have a reliable car to get there.
“It’s scary because I have to have a C-section. So if I were to go into labor here, there'd be nothing they can do for me until I got to Mason City,” Grover said.
Grover also doesn’t have a reliable car.
“It's a little scary not knowing if I’m going to have time to get there," she said. "Or if something happens, I'm gonna have to go by an ambulance."
‘The right thing to do’
About two hours southeast of Iowa Falls, Compass Memorial Hospital, located in the small town of Marengo, is bucking the trend. It’s in the process of finishing a new labor and delivery unit.
CEO Barry Goettsch said the hospital is aiming to open the unit with two birthing suites by the end of next year. It’s projecting to have between 150 and 175 births a year.
Goettsch said Compass Memorial shut down its previous unit in the 1980s, and local women have to drive to the nearby cities of Iowa City or Cedar Rapids to give birth.
“The people who live in our area deserve the best, and they shouldn't have to drive 45 minutes or further to get the perceived best from somebody bigger” Goettsch said.
To help attract enough expectant mothers, the hospital designed the birthing suites to be more upscale, he said.

Compass Memorial CEO Barry Goettsch stands in one of the hospital’s new birthing suites. Goettsch says the hospital is expected to lose $1 million annually on the service but thinks it's important to have.
“We have a queen-size bed in the wall, and that then pulls down and there's a sofa couch, and so it kind of converts into more of a hotel-type room for the remainder of their stay,” Goettsch said.
Compass Memorial expects to confront a lot of the issues that the Iowa Falls hospital faced.
Marengo, which has a population of about 2,400, is also an aging community, Goettsch said half of the town’s births will likely be Medicaid-funded, and the hospital will lose $1 million a year to operate the unit.
Plus, he said they haven’t even started searching for an OB/GYN, which will be difficult as Iowa faces a shortage of OB/GYNs, particularly in rural areas.
Still, Goettsch called opening the unit “the right thing to do.”
“That's the nature of health care,” he said. “I mean, if we're not doing what's right, and we're not doing the best we can for the folks that utilize our organization, then we kind of missed the point of being in health care.”
This story was produced by Side Effects Public Media, a news collaborative covering public health.
This report is part of a collaborative project titled Seeking a cure: The quest to save rural hospitals. It includes the Institute for Nonprofit News and INN members IowaWatch, KCUR, Bridge Magazine, Wisconsin Watch, Side Effects Public Media and The Conversation; as well as Minnesota Public Radio, Iowa Public Radio, Wisconsin Public Radio, The Gazette (Cedar Rapids, IA), Iowa Falls Times Citizen and N'west Iowa Review. The project was made possible by support from INN, with additional support from the Solutions Journalism Network, a nonprofit organization dedicated to rigorous and compelling reporting about responses to social problems. For more stories visit hospitals.iowawatch.org.

